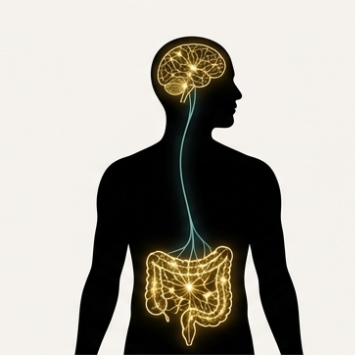
"the second brain"
How Can You Heal Your Gut to Transform Your Mental Health?
CONSCIOUSNESS & SCIENCE
11/4/20259 min read


How Can You Heal Your Gut to Transform Your Mental Health?
You hold your stomach when you're nervous. You feel butterflies before something exciting. You lose your appetite when grief strikes. Your body has always known what science is only now beginning to prove: your gut and your brain are not separate territories. They are ancient allies, speaking in a language older than words.
The conversation between your intestines and your mind happens through trillions of whispered messages every single day. When this dialogue flows smoothly, you feel grounded, clear, emotionally resilient. When it breaks down—when your gut becomes inflamed, depleted, or overrun with the wrong microbial residents—your mental health pays the price. Anxiety creeps in. Depression settles like fog. Your thoughts become slower, heavier, harder to navigate.
This is not metaphor. This is not ancient mysticism. This is the microbiota-gut-brain axis—and it's one of the most revolutionary discoveries in modern neuroscience.
The Science of Your Second Brain
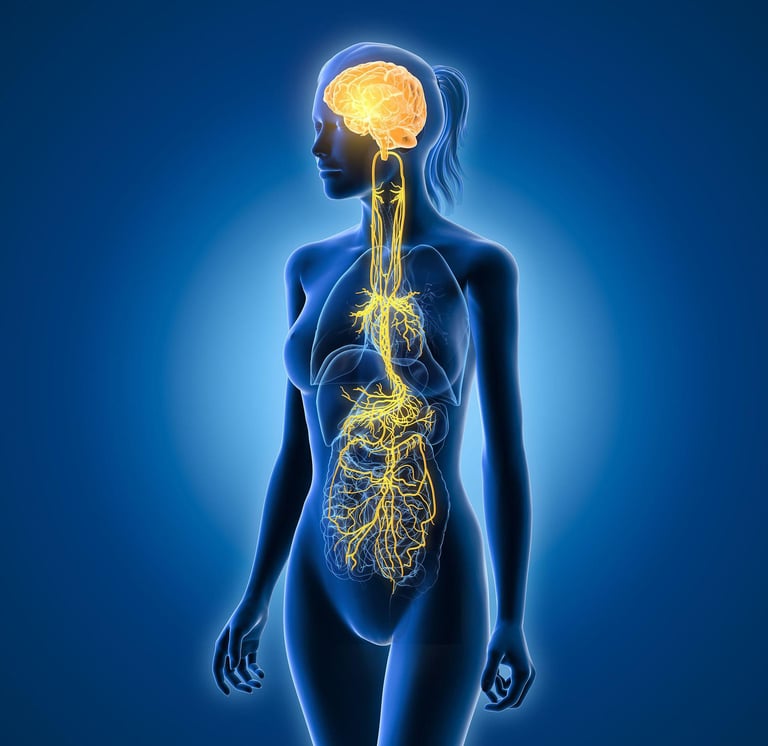
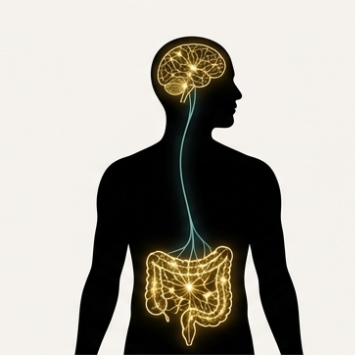
Your gut affects your mood, your sleep, even your motivation to exercise Stanford Medicine. This happens through a communication network so intricate that scientists now call your gastrointestinal tract "the second brain." Your intestinal walls contain nearly 170 million neurons—more than your spinal cord. These neurons are in constant, bidirectional conversation with the brain in your skull, primarily through the vagus nerve: a wandering superhighway of electrical signals that connects your belly to your mind.
But the neurons are only part of the story. Probiotics significantly regulate gut microbiota, which is vital for digestion, metabolism, immune function, and mental health MDPI. The trillions of bacteria, viruses, and fungi living in your intestines—collectively called your microbiome—produce chemicals that directly influence brain function. They manufacture neurotransmitters. They modulate inflammation. They create compounds that either protect your neurons or slowly erode them.
When animals are raised without any gut bacteria at all, they develop brain abnormalities Frontiers. Their neural architecture changes. Their behavior shifts. The absence of these microscopic partners literally reshapes the brain. This tells us something profound: we are not separate from the microbes within us. We are ecosystems.
The Vagus Nerve: Your Body's Information Superhighway
The vagus nerve is the physical embodiment of the gut-brain connection. This single cranial nerve—the longest in your body—extends from your brainstem down through your chest and into your abdomen, touching nearly every major organ along the way. It carries signals in both directions: your brain tells your gut how to respond to stress, and your gut tells your brain what's happening in the microbial world below.
Vagus nerve signaling from the gut alleviates anxiety and depressive-like states while promoting motivational and memory functions PubMed. When you eat a nourishing meal, gut-originating vagal signals fire upward, delivering messages of safety and satisfaction to your brain. This is why food can be genuinely comforting—not just emotionally, but neurologically.
The research on this is striking. A yearlong randomized clinical trial of 493 adults found vagus nerve stimulation therapy led to improvement in depressive symptoms, ability to complete daily tasks, and quality of life Brainstimjrnl. While this study used electrical stimulation devices, it points to a larger truth: strengthening vagal tone through natural means—deep breathing, meditation, singing, cold exposure—can enhance the gut-brain dialogue and improve mental well-being.
The vagus nerve doesn't just carry abstract signals. It functions as an anti-inflammatory pathway, with proven effects for treating depression PubMed Central. When vagal activity is strong, it dampens systemic inflammation—the kind that contributes to both gut disorders and psychiatric conditions. When vagal tone is weak, inflammation runs unchecked, creating a biological environment where anxiety and depression thrive.
This is the bridge between your digestion and your disposition. Between what you eat and how you feel. Between the soil of your belly and the garden of your mind.
The Microbial Architects of Mood
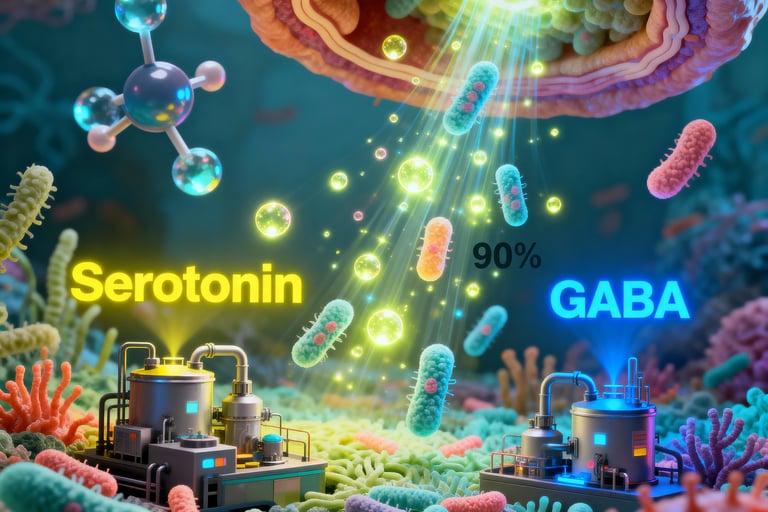
Your gut bacteria do more than digest food. They are biochemical factories, producing substances that profoundly affect your emotional state. Among the most important are neurotransmitters—the same chemicals that psychiatric medications attempt to regulate.
Your intestinal microbes produce serotonin, the neurotransmitter associated with happiness and emotional balance. In fact, approximately 90% of your body's serotonin is manufactured in your gut. They produce GABA, the brain's primary calming agent. They produce dopamine, which governs motivation and reward. When your microbial community is diverse and balanced, these neurotransmitters flow freely. When it's depleted or imbalanced, production falters.
But perhaps the most important compounds your gut bacteria create are short-chain fatty acids (SCFAs)—particularly acetate, propionate, and butyrate. These molecules are produced when beneficial bacteria ferment dietary fiber in your colon.
SCFAs cross the blood-brain barrier and have a pivotal impact on microbiota-gut-brain crosstalk, mediating behavioral and neurological processes PubMed Central. They're detectable in human cerebrospinal fluid, meaning they directly bathe your brain in microbial metabolites. Patients with major depressive disorder show lower baseline levels of butyrate and propionate, with higher butyrate levels associated with greater likelihood of remission PubMed.
This is not subtle. Butyrate reduces neuroinflammation, supports the growth of new neurons, and protects the integrity of the blood-brain barrier—the fortress that keeps toxins out of your central nervous system. Butyrate influences protein aggregation associated with neurodegenerative diseases, supports gut-brain communication through neurotransmitter release modulation, and impacts mood, behavior, and brain function Springer.
When you nourish the bacteria that produce these compounds, you are literally feeding your mental health from the inside out.
The Inflammation Connection
Depression and anxiety are not purely psychological phenomena. Increasingly, researchers understand them as inflammatory conditions—disorders where the immune system has gone haywire, flooding the body and brain with inflammatory signals that disrupt normal function.
The gut-brain axis operates as a bidirectional communication pathway where gut microbiota regulates the central nervous system via immune, neuroendocrine, and vagal pathways Nature. When your gut becomes permeable—a condition sometimes called "leaky gut"—undigested food particles, bacterial fragments, and toxins slip through the intestinal barrier into your bloodstream. Your immune system perceives this as an invasion and launches an inflammatory response.
This inflammation doesn't stay localized. It travels. It crosses the blood-brain barrier. It activates microglia, the immune cells of your brain, which then release inflammatory molecules called cytokines. These cytokines interfere with neurotransmitter production, disrupt neural connections, and create the biological signature of depression: fatigue, brain fog, low motivation, flattened mood.
Healing the gut reduces systemic inflammation. Restoring microbial balance calms the immune system. Strengthening the intestinal barrier protects the brain. The path to mental clarity may begin not with a prescription, but with a plate.
Three Science-Backed Ways to Support Your Gut-Brain Axis Today
1. Feed Your Beneficial Bacteria with Fiber-Rich Foods
Your gut bacteria need fuel, and their preferred food is dietary fiber—the indigestible plant material found in vegetables, fruits, whole grains, legumes, nuts, and seeds. When bacteria ferment this fiber, they produce those crucial short-chain fatty acids that support brain health.
Aim for a diversity of plant foods. Each type of fiber feeds different bacterial species, and microbial diversity correlates with mental resilience. Include:
Prebiotic-rich vegetables: Garlic, onions, leeks, asparagus, Jerusalem artichokes
Resistant starches: Cooked and cooled potatoes, oats, green bananas
Legumes: Lentils, chickpeas, black beans
Whole grains: Oats, quinoa, barley
Colorful vegetables: The more variety, the better
The standard American diet provides about 15 grams of fiber daily. For optimal gut-brain health, aim for 30-40 grams. This shift alone can transform your microbial landscape within weeks.
2. Incorporate Fermented Foods Regularly
Fermented foods harness the potential to modulate the microbiota-gut-brain axis for mental health through whole food supplementation strategies PubMedScienceDirect. These ancient foods—preserved through bacterial fermentation—deliver live beneficial microorganisms directly to your gut.
Fermented vegetables led to reduction in anxiety-like behaviors and stress hormone levels in animal models Springer. While human research is still emerging, the preliminary evidence is compelling. Fermented foods support microbial diversity, reduce inflammation, and may directly influence mood.
Include these regularly:
Unsweetened yogurt with live active cultures (look for Lactobacillus and Bifidobacterium strains)
Kefir, a fermented milk drink richer in probiotics than yogurt
Sauerkraut (raw, not pasteurized—heat kills beneficial bacteria)
Kimchi, the spicy Korean fermented vegetable dish
Miso, fermented soybean paste used in soups and marinades
Kombucha, fermented tea (choose low-sugar varieties)
Start small—a few tablespoons daily—and gradually increase. Your gut needs time to adjust to new microbial residents.
3. Activate Your Vagus Nerve Through Daily Practices
You don't need an implanted medical device to strengthen vagal tone. Simple, accessible practices can enhance gut-brain communication naturally:
Deep, diaphragmatic breathing: Slow belly breaths activate the parasympathetic nervous system and stimulate the vagus nerve. Practice 5-10 minutes of 4-7-8 breathing (inhale for 4, hold for 7, exhale for 8) daily.
Cold exposure: Brief cold showers or face dunks in ice water trigger the "dive reflex," which strongly activates vagal pathways. Start with 30 seconds of cold water at the end of your shower.
Humming, singing, or chanting: The vagus nerve innervates your vocal cords. Creating sound vibration mechanically stimulates the nerve. Sing in the car. Hum while cooking. Try "Om" meditation.
Gentle yoga or tai chi: Slow, mindful movement with focused breathing enhances vagal activity while reducing stress hormones.
Meditation and mindfulness: Regular meditation practice increases heart rate variability—a marker of healthy vagal tone—and reduces inflammation.
These practices don't just feel calming—they are calming, at a physiological level, enhancing the dialogue between your gut and brain.
The Bigger Picture: Trusting the Wisdom of Your Body
Modern psychiatry often treats the mind as software running on the hardware of the brain, isolated from the rest of the body. The gut-brain axis research reveals how insufficient this model is. Your mental health is inseparable from your digestive health, your immune health, your microbial health. You are not a brain with a body attached. You are an integrated ecosystem where every system influences every other.
This knowledge is empowering. It means you have agency. While you cannot directly control neurotransmitter release in your brain, you can influence the microbial community that produces neurotransmitter precursors. You cannot manually reduce neuroinflammation, but you can heal your gut lining and calm your immune system. You cannot consciously regulate your vagus nerve, but you can practice breathwork, cold exposure, and meditation that strengthen vagal tone.
The question is not whether your gut influences your mental health—the science on that is settled. The question is: What will you do with this knowledge?
Frequently Asked Questions
How long does it take to see mental health improvements from gut healing?
Microbial changes can begin within 24-48 hours of dietary shifts, but noticeable mental health improvements typically emerge over 4-8 weeks. The gut lining regenerates every 3-5 days, but establishing stable microbial populations and reducing chronic inflammation takes longer. Consistency matters more than perfection.
Can gut healing replace psychiatric medication?
For some people with mild to moderate symptoms, dietary and lifestyle interventions may be sufficient. However, gut-brain axis support should be viewed as complementary to—not replacement for—conventional treatment. If you're currently taking psychiatric medication, work with your healthcare provider. Many people find that addressing gut health allows them to optimize medication dosages or enhance treatment effectiveness.
What if I have digestive symptoms along with anxiety or depression?
This is extremely common and often indicates that gut dysfunction is contributing to your mental health challenges. Conditions like IBS, SIBO, and inflammatory bowel disease frequently co-occur with anxiety and depression. Addressing the root cause—gut dysbiosis, intestinal permeability, or inflammation—often improves both digestive and psychological symptoms simultaneously.
Are probiotic supplements necessary, or is food enough?
Food should be your foundation. Fermented foods and fiber-rich plants provide a broader spectrum of beneficial compounds than any supplement. That said, specific probiotic strains have shown promise for particular conditions in research settings. If you choose to supplement, look for products with strains that have clinical evidence (such as Lactobacillus helveticus and Bifidobacterium longum for mood support) and at least 10-20 billion CFUs per dose.
How do I know if my gut-brain connection is impaired?
Common signs include: digestive issues (bloating, irregular bowel movements, food sensitivities) alongside mental health symptoms; mood fluctuations that seem connected to meals; brain fog, especially after eating; chronic fatigue; heightened anxiety or irritability for no clear reason. If you experience multiple symptoms, addressing gut health may be particularly beneficial.
The Path Forward
The emerging science of the gut-brain axis is not asking you to abandon your current approach to mental wellness. It's inviting you to expand it. To recognize that healing happens on multiple levels—neurological, microbial, immunological, emotional—and that these levels are not separate but woven together.
Between the ancient yogis who spoke of digestive fire influencing consciousness and the modern neuroscientists measuring neurotransmitters in the gut, there is no contradiction. There is convergence.
Your gut has been speaking to your brain since before you were born—shaping your stress response, influencing your emotional baseline, contributing to the very architecture of your nervous system. Now, for perhaps the first time in your life, you can consciously participate in that conversation.
Feed the garden within you. Strengthen the bridge between your belly and your mind. Trust that when you heal your gut, you create the biological conditions for a clearer, calmer, more resilient state of being.
This is not a miracle cure. It is something better: a return to the fundamental interconnectedness your body has always known.









Connect
© 2025. All rights reserved.
info@cosmiclifeflow.com
